Gum health: Causes and mechanisms

Recognising the causes of periodontal disease and gingivitis1,2
Take a closer look at the causes and mechanisms behind the condition, with a particular focus on why poor oral hygiene is the major cause of periodontal disease1,2
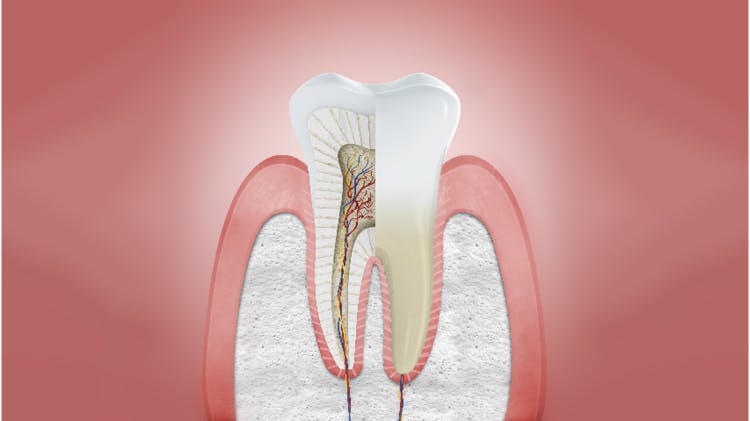
Periodontal disease is caused by plaque1–4
- Periodontal disease is caused by bacteria at the gum margin forming plaque on the dental pellicle1,3
- Endotoxins and bacterial debris released by these plaque bacteria cause inflammation in the surrounding gum known as gingivitis1,2,4
- If plaque is not removed, over time this inflammatory response can become chronic periodontitis, leading to progressive tissue destruction1,2
Progression of gingivitis and periodontal disease
Gingivitis is a reversible condition that develops from healthy gums when plaque around the gum line induces inflammation of the gingivae. If left untreated, chronic gingival inflammation can progress into chronic periodontitis, causing irreversible destruction of the periodontal tissues. While not all gingivitis becomes progressive, almost half of adults are susceptible.2
Healthy gums
Uninflamed gingivae without any of the signs of periodontal disease. Characteristics include:
- Pale pink and firm gingivae
- Stippled
- Firmly attached to teeth
- Knife-edge margin
- Not normally prone to bleeding on brushing or probing

Gingivitis
Reversible plaque-induced inflammation of the gingivae.2Characteristics include:
- Change in colour of the gingivae
- Marginal gingival swelling and blunting of the gingival papillae
- Bleeding on probing and brushing
- Probing depth of gingival crevice does not exceed 3mm
- Gingival attachment remains unchanged

Chronic periodontitis
Irreversible destruction of the periodontal tissues caused by chronic inflammation.2 Characteristics include:
- Gingivae appear inflamed
- Bleeding on probing and brushing
- Destruction of junctional epithelium and loss of gingival attachment (true pocketing and recession)
- Alveolar bone loss
- Tooth mobility and drifting
Other periodontal conditions
The current classification system of periodontal disease
Developed in 1999 at the International Workshop for Classification of Periodontal Conditions, the current classification system of periodontal disease is based on eight categories.2 A new classification workshop was held in late 2017; the consensus from this meeting is set to be published in 2018.2
| The main disease categories in the current periodontal classification | |
| 1 | Gingival disease |
| 2 | Chronic periodontitis |
| 3 | Aggressive periodontitis |
| 4 | Periodontitis as a manifestation of systemic disease |
| 5 | Necrotising periodontal disease |
| 6 | Abscesses of the periodontium |
| 7 | Periodontitis associated with endodontic lesions |
| 8 | Developmental or acquired deformities and conditions |
Table adapted from British Society of Periodontology, 20162
Risk factors for periodontal disease can be divided into two categories2
Modifiable risk factors
Local
- Plaque and calculus2,5
- Wearing partial dentures2
- Deficient dentition including open contacts and overhanging and poorly contoured restorations2,5
- Anatomical factors including malpositioned teeth, furcations, root grooves and concavities, and enamel pearls2,5
Systemic
- Poor oral hygiene2
- Smoking and tobacco2
- Stress2
- Poor nutrition2
- Diabetes mellitus (poorly controlled)2
- Taking medications that cause xerostomia2
Targeting modifiable risk factors, such as poor oral hygiene, can improve gum health management and treatment outcomes
Non-modifiable risk factors
- Family history and genetic factors2,5
- Some hormonal variations, e.g. during puberty, pregnancy and menopause6
- Underlying immunodeficiency2,5

Patient barriers to maintaining gum health
Hard-to-reach areas
- Any irregularity that makes tooth cleaning difficult can encourage the accumulation of plaque,5,7 including:
- Malpositioned teeth5
- Overhanging edges on fillings5
- Poorly contoured fillings5
- Some types of dentures5
- Calculus (tartar) formation may cause plaque retention5
Patients ignore symptoms and professional advice
The early symptoms of gum disease may be ignored for a number of possible reasons:
- Lack of awareness of gum health importance (believing bleeding gums to be ‘normal’)
- A belief that teeth are more important than gums
- More focus on current cosmetic issues rather than on possible future issues caused by periodontal disease
- Expect dental practitioner to fix gum issues instead of proactively managing own gum health
Help your patients on their journey to optimal gum health
Impact on patient quality of life
Find out about the impact periodontal disease has on patients’ daily lives



